Scientists add some bizarre things to vaccines, such as aluminium and extracts from shark livers. Many vaccines simply don’t work without them – but no one knows why.
In 1925, Gaston Ramon embarked upon an experiment that even he described as… “interesting”.
A few years earlier, the French veterinarian had been trying out a new diphtheria vaccine on horses, when he made an accidental discovery: some animals reacted by developing nasty abscesses at the injection site, and these ones also tended to develop stronger immune responses. This got him thinking – what else could he add to the vaccine, to encourage this to happen?
Over the next year, Ramon tested a bizarre smorgasbord of ingredients, seemingly based on what he happened to have in his kitchen cupboards. Together with the diphtheria vaccine, his unfortunate patients were injected with tapioca, starch, agar, lecithin – an emulsion of oil, commonly found in chocolate – and even breadcrumbs.
The experiments were a success. Animals which had been given vaccines that included Ramon’s concoctions produced significantly more antibodies than those which didn’t, suggesting that they would be better protected against diphtheria.
And thus the field of “adjuvants” was born. Named after the Latin word “adjuvare”, meaning “to help” or “aid”, these are substances which can be added to vaccines to make them more effective. They’re widely used to this day – and they’re no less weird than they were to begin with.
The most commonly used adjuvant on the planet is aluminium. The chemical is found in the majority of vaccines, including the diphtheria, tetanus, and whooping cough (DTP) vaccine, as well as those that protect against hepatitis A, hepatitis B, HPV, Japanese encephalitis, meningitis B, anthrax, pneumococcus, and Haemophilus influenzae type b.
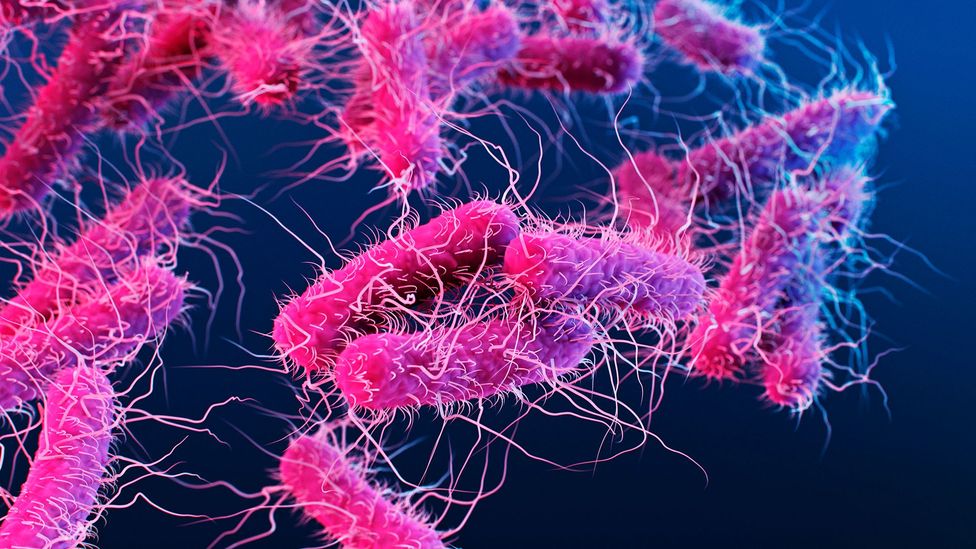
Other popular adjuvants include squalene, an oily substance made from shark livers, and extracts from the bark of the quillaja tree, which has traditionally been used by the Andean Mapuche people to make soap as its bark can be powdered and mixed with water to form a lather. The newest additions – which haven’t yet been licensed – are perhaps the strangest of all, such as the disembodied tails of bacteria and “bacterial ghosts”, made from their empty skins.
It’s been estimated that vaccines save two to three million lives per year, as well as preventing lifelong disabilities. No one has quantified exactly what proportion of these triumphs are down to adjuvants. But by encouraging the body to respond to vaccines more vigorously, they can make them more effective and protect people for longer than they otherwise would. In some demographics, such as the elderly, certain vaccines simply wouldn’t work without them.

“Without an adjuvant, antibodies will generally disappear, maybe after a few weeks or months. But with adjuvants they might last for a few years.” says Bingbing Sun, a chemical engineer at Dalian University of Technology, in the Chinese city of Dalian. He gives the example of certain types of hepatitis B vaccine. “If they don’t include adjuvants, antibody production will be very, super low. They don’t really have the ability to induce antibody production,” he says.
For over a century, why these apparently random ingredients are so essential to vaccines has remained a total mystery. Now scientists are racing to unravel their secrets.
A mistaken scandal
First up, though the concept of additives in vaccines might sound alarming, they’re included in microscopic quantities. There is as little as 0.2mg of aluminium in a typical vaccine dose, which is equivalent to less than the weight of a single poppy seed. The weight of evidence is that adjuvants do not lead to serious side-effects.
In fact, safety is the reason adjuvants were popularised in the first place.
Back in the 1970s, a paediatric neurologist gave a speech at the Royal Society of Medicine which caused controversy that lasted a decade. John Wilson claimed that 36 children had acquired brain damage – and erroneously blamed it on the vaccine for pertussis.
The story was picked up by journalists, and before long it was a full scandal – complete with prime-time specials and front page headlines. Over the coming years, the rates of pertussis vaccination plummeted by more than half in the UK, while in some countries it stopped altogether.
None of it was true – the vaccine had been widely administered for decades without incident. But the vaccine did produce some mild immediate side-effects, such as a fever, and this was easy to confuse with something more sinister. In the end, the scandal spurred scientists to look for new ways to make vaccines.
Previously, most vaccines had been made using live microorganisms, which had been weakened in some way to make them less infectious or harmful – while still helping the body to recognise them – or killed and included whole. The latter was the case for the pertussis vaccine, which was administered along with tetanus and diphtheria (DTwP).

These vaccines were sometimes accompanied by temporary symptoms because they mimicked natural infections. And just like natural infections, they were highly effective at generating immunity – often giving rise to potent responses which would last decades. Many vaccines containing live microorganisms also provided a kind of accidental bonus protection against unrelated infections, which continues to benefit people to this day (Read more about the mystery of why some vaccines are doubly beneficial).
The new system was different. After the pertussis scare, scientists started to favour just including certain parts of microorganisms, such as the toxins they produce or fragments from their outer surfaces. These new vaccines were just as safe and much more comfortable to receive. But there was a catch.
Making vaccines this way means they are less “immunogenic” – the protection they provide isn’t as robust and it doesn’t last as long. To overcome this, scientists turned to adjuvants.
The aluminium paradox
Aluminium is not only the most common adjuvant, but one of the oldest.
Shortly after Ramon discovered that his horses responded better to vaccines with added culinary ingredients, the British immunologist Alexander Glenny made another accidental finding. In 1926, his team was trying to purify the toxin produced by the diphtheria bacteria, to make it dissolve less rapidly in the body. The hope was that this would mean it lingered for longer at the injection site, and produced a stronger immune response.
To achieve this, Glenny tried using aluminium salts which, legend has it, just so happened to be the first thing he saw in his chemical shelf – who knows, perhaps it was alphabetised. But when he vaccinated guinea pigs with his freshly-prepared diphtheria toxin, something unexpected happened. Those which had been injected with the toxin plus aluminium salts developed much stronger immunity than those which were only injected with the toxin, and not because it was more pure. They were responding to the aluminium itself.
To this day, the aluminium in vaccines is always in the form of salts. These include aluminium hydroxide (commonly used as an antacid to relieve indigestion and heartburn), aluminium phosphate (often used in dental cement) and potassium aluminium sulphate, which is sometimes found in baking powder.
Genny himself believed that aluminium salts help by binding to the vaccine’s main ingredient, the part resembling the pathogen, presenting it to the immune system more slowly. This might give the immune system longer to respond, and therefore lead to stronger immunity.
But this idea has gone out of fashion – and the truth has proven to be a lot more complicated.
One theory is that the toxicity of aluminium salts is, paradoxically, the reason they work. They lead distressed cells to release uric acid, which activates an immune reaction normally associated with damage. Immune cells flock to the site, and start producing antibodies – and voila, the vaccine has worked.
Another idea is that a receptor called “Nalp3” is likely to play a central role. For a 2008 study led by Richard Flavell from Yale University, Connecticut, mice which had been genetically engineered without it were injected with a vaccine containing aluminium. Their immune response was almost non-existent. However, when they tried a vaccine using a different adjuvant – one containing an emulsion of mineral oil – the animals produced antibodies as usual.

This suggests that in ordinary mice (and humans), the aluminium in vaccines works by activating the Nalp3 receptor, which acts as a kind of danger switch alerting the rest of the immune system. Once the immune cavalry has arrived, they help to generate a stronger response and the vaccine has more of an impact.
In fact, though there are many different types of adjuvant, and many different potential mechanisms, this seems to be at the core of how they work – they attract the attention of the immune system, and this leads to a stronger memory of the pathogen the vaccine resembles.
Take squalene, an oil made from shark livers and a key ingredient in the adjuvant “MF59”. It’s already added to vaccines for the seasonal flu and is currently being investigated for use in vaccines against Covid-19. (This has caused some controversy, after reports that, if such a vaccine were mass produced so that the entire global population could receive a dose, around 250,000 endangered sharks would need to be slaughtered – however this estimate is up for debate.)
One way MF59 is thought to work is by triggering the release of chemokines – signalling chemicals – by nearby cells, which then encourage other cells to produce yet more chemokines. Eventually, this cascade attracts immune cells, which ingest the vaccine – including recognisable parts of the pathogen it protects against – and transport the lot to the lymph nodes, which filter pathogens out of the body and help to identify infections.
The next generation
“In the vaccine industry, people are very conservative,” says Sun. “So whenever they try to find an adjuvant for a new type of vaccine, most of the ones under investigation are the traditional ones, which we know are safe and effective.”
However, scientists are starting to wonder whether they can come up with something better than those accidental adjuvants from the 1920s and 1950s, discovered before the structure of DNA was known, or man had set foot on the Moon, when computers either didn’t exist or were the size of a house.
This is particularly important, because of a tragic irony: people who are the most vulnerable to infections also tend to have the weakest responses to vaccines. For example, one flu vaccine was 58% effective at preventing hospitalisation in “frail” people over the age of 65, but 77.6% effective in those who were not.
There are already fears that this could be the case for vaccines against Covid-19, which is hundreds of times more likely to kill a person over the age of 80 than those under the age of 50. (Learn more about why older people are harder to vaccinate.)
As the global population of septuagenarians, octogenarians, nonagenarians and centenarians creeps up, these problems are only set to get worse. Enter the next generation of adjuvants, which promise to make modern vaccines even more effective.
One candidate is the protein flagellin. It’s found in bacteria such as Salmonella, which use it in their tails, or flagella, to propel themselves around. Sometimes it’s made by detaching the tails from bacteria – though more recently it’s become common to grow it in genetically modified cells.
Flagellin isn’t yet licensed for use in any human vaccine, but it’s shown promising results in trials.
During a natural infection with bacteria, the protein binds to receptors on the surface of immune cells. This acts like a danger signal and encourages them to tell other immune cells to flock to the site – leading to a protective response. In theory, this is also what happens when it’s included in vaccines. As with other adjuvants, it gets the attention of the immune system, so that the vaccine can do its job.
So-called bacterial ghosts are another possibility, composed of the empty skins of bacteria. These are made by splitting open bacterial cells, such as those belonging to E. coli, so that you are left with the cell membrane and nothing else. Like squalene-based adjuvants, they lead to the production of chemical signals, which call for help from immune cells and maximise the chances of them finding the vaccine.
“The development of adjuvants is tedious work,” says Sun. “I mean, you have to make sure of the safety as well as the efficacy – and this takes time. For a traditional vaccine, it usually takes about 10-12 years for us to licence the vaccine.”
Who knows, nearly a century after Gaston Ramon experimented with breadcrumbs, the world of adjuvants might be about to get a modern makeover – and the next generation looks set to be just as bizarre as they were to begin with.
The paragraph about adjuvants and possible side effects has been amended for clarification.





